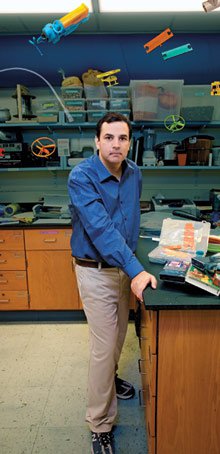
José Gómez-Márquez's lab at MIT seems to be part toy store, part machine shop, and part medical center. Plastic toys are scattered across the bench tops, along with a disassembled drugstore pregnancy test, all manner of syringes, and a slew of fake body parts. Coffee filters have been transformed into paper-based diagnostics; a dime-store helicopter provides the design for a new asthma inhaler; even a toilet plunger has been put to use, rigged with tubes and glue to form a makeshift centrifuge.
"Centrifuges break down all the time," says Gómez-Márquez, spinning the plunger's wooden handle in his hands. That's a problem for health-care workers, because even simple medical tests rely on the devices to separate molecules in a blood or urine sample. In rich countries, the broken equipment is quickly repaired or replaced; in the poor countries where Gómez-Márquez often works, finding replacement parts can be impossible, rendering the equipment useless. So he's tried to use readily available materials to make simple versions that are either easy to fiddle with, disposable, or unlikely to break in the first place. "This one could work even without power," he says of the plunger-cum-centrifuge.
Gómez-Márquez, a native of Honduras, is a talented tinkerer: "My mother used to say my toys would last only a few days because I would take them apart, saying I had detected a defect," he recalls. But he is also an inventor on a mission. "When you grow up in a developing country," he says, "you get the sense that fancy technology is expensive to replace, so it often doesn't get replaced."
In his few short years in the field, Gómez-Márquez has gained a reputation among Boston medical-device researchers for his insight into a wide array of design issues. "There are not many people out there that have as broad a view of innovative technology in low-resource settings," says Kristian Olson, a physician at Massachusetts General Hospital in Boston and leader of the Global Health Initiative at the Center for Integration of Medical and Innovative Technology. "He finds a need and then a technology to fit that need. It's a remarkable way of approaching technology development for poor people."
Some might say that Gómez-Márquez was born to improve medical technology. In 1976, when prenatal ultrasound was not available to his mother's doctor in Honduras (it was just catching on in the United States), the physician mistakenly concluded that she was carrying twins and miscalculated how far along she was in her pregnancy. She was induced to give birth in what was actually her seventh month, and Gómez-Márquez--no twin in sight--was born with the numerous health concerns typical of an underweight and premature infant. He escaped any long-term damage. But thanks to a childhood spent in and out of doctors' offices, he developed a profound sense of how important health care was, how capricious access to it could be, and how much medical devices could do to improve it.
It helped, too, that he comes from a medical family. His grandfather, a surgeon, worked at both private and public hospitals in Tegucigalpa, the capital of Honduras, where Gómez-Márquez saw firsthand the differences that money made in access to medical services. Poor people, who went to the public hospital, were less likely to get chemotherapy or appropriate prostheses. "People who could afford it would go to Texas or Boston for their health care," he says.
$$PAGE$$
Gómez-Márquez left Honduras in the late 1990s to attend college in the United States. But his education was sidetracked by Hurricane Mitch, which devastated Honduras in 1998. With his parents in Tegucigalpa no longer able to help pay his tuition, he began working a variety of jobs to support himself--"sometimes the late shift, sometimes regular shifts, sometimes cool stuff, and sometimes humbling stuff." He eventually ended up at Worcester Polytechnic Institute in Massachusetts. "Quite frankly, it was very hard," he says. "I wouldn't recommend that path to anyone."
What little free time he had was devoted to his real interest--combining aspects of different technologies to make them do new things. In 2005, the fledging inventor joined a team participating in MIT's IDEAS competition, which aims to develop new technologies or programs that will have a positive impact on the world. His team focused on developing technologies for health care, inspired by a call from the World Health Organization (WHO) for new ways to deliver the measles vaccine; the disease, though nearly eradicated in the United States, still kills 500 people a day worldwide, mostly children. Gómez-Márquez and his coworkers decided to develop a needle-free system for use in poor countries.
Administering injectable vaccines takes training, and his team wanted "a device that would allow any community health-care worker, rather than a trained nurse, to give a dose of vaccine," Gómez-Márquez says. While needle-free vaccination systems already existed, most relied on aerosolization technology that is cumbersome and requires electricity.
After examining prototypes of new kinds of devices from drug delivery and engineering firms, Gómez-Márquez quickly decided that existing approaches were much too complicated. "The device was sitting in a fancy box in eggshell foam," he says of one prototype he studied. "If it needs foam to survive a trip to New England, it's never going to make it to Central America."
Taking inspiration from the disposable cartridges used in ink-jet printers, Gómez-Márquez's team designed individual vaporizers preloaded with the correct dose of vaccine; the devices could be used once and then thrown away. The team also developed a way to stabilize the vaccine within the cartridges, eliminating the need for cold storage. Other researchers who've worked on vaccine nebulizers have tried to modify asthma nebulizers, which are not disposable or cheap. "If the aerosolizing head broke, the machine had to be sent back," Gómez-Márquez says. "In our case, because it's just 10 cents, you can throw the broken one away and pull another one out of the box." Most nebulizers also require a power source to run the compressor, which converts liquid medicine into vapor. Gómez-Márquez's team made sure their system can be powered by multiple sources, such as a foot pump, when electricity isn't available.
The resulting device won an Award for International Technology at the IDEAS competition in 2006. "That gave me the idea that I could really do this for a living," Gómez-Márquez says. The team is still improving the device, with funding from the U.S. National Institutes of Health.
$$PAGE$$
Gómez-Márquez and a team entered the IDEAS competition again the next year, this time focusing on strategies to improve drug compliance in tuberculosis treatment. Though TB can be treated with antibiotics, the disease killed 1.8 million people in 2007, according to WHO estimates, and 9.3 million new cases were diagnosed the same year. One of the biggest challenges in treating TB is making sure that patients stick with the lengthy course of medication required to clear the infection from the body.
A number of new technologies for monitoring drug compliance are being tested, but most of them rely to some degree on self-reporting; for example, patients may be given a phone number to call when they've taken their medicine. "I was the cynic," says Gómez-Márquez. "Patients had no incentive to tell us if they didn't take their drugs." His team developed a simple paper-based test that can be used in conjunction with an incentive program. The test strip is made from layers of coffee filters impregnated with chemicals that react with metabolites of the TB drug in urine, revealing a unique code. The patient texts the code to a central database every day to earn cell-phone minutes. The team launched a trial of the system in Karachi, Pakistan, earlier this year.
Amy Smith, cofounder of the International Development Initiative at MIT, was so impressed with Gómez-Márquez that she hired him to run the Innovations in International Health program, also at MIT, in 2007. He has since built a network of collaborators in countries around the world who can tell him about their populations' health-care needs. That kind of consultation, which lies at the heart of Gómez-Márquez's philosophy, reflects a growing trend in the field of appropriate technology: collaborating early on with the people who will use the devices. "José is really at the forefront of that," says Catherine Klapperich, director of the Biomedical Microdevices and Microenvironments Laboratory at Boston University. "Who is the customer, what do they want, what are they willing to use? You can't assume the answers--that's one of the things José teaches his students and his colleagues."

No toys: Gómez-Márquez is working on a number of new inhaler technologies for use in poor countries. A disposable cartridge for inhalable vaccine (top left) could make it easier to inoculate children against measles. A plastic helicopter (top right) inspired a new approach to delivering asthma medicine to children. And a paper spacer (center) to use with inhalers provides an easy and disposable way to get more medication into the lungs.
Credit: Steve Moors
Gómez-Márquez aims to push this approach even further by encouraging physicians and scientists in poor countries to design their own devices. He is now creating development kits for medical technology--sort of like Erector sets for medical professionals--which will initially be used in Nicaragua. The kits will enable doctors and medical students to devise diagnostics, drug delivery devices, microfluidic chips, and more.
At least, that is the theory. But will busy medical professionals find the kits helpful? Are they too complicated to use or--conversely--too simple to yield useful technology? Gómez-Márquez and his students brought some to Nicaragua over the summer to find out. His hope is that the kits will help a new culture of invention take root. In the long term, it's this kind of approach that could truly revolutionize both medical care and technology in poor countries. --Emily Singer